Exacerbations (Studies I-II)
CINQAIR consistently helped prevent exacerbations vs placebo in multiple clinical trials over 52 weeks1,2
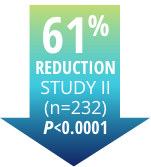
Reduction in
overall exacerbations
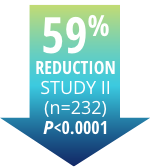
- Study I: 50% exacerbation reduction over 52 weeks (n=245, P<0.0001)
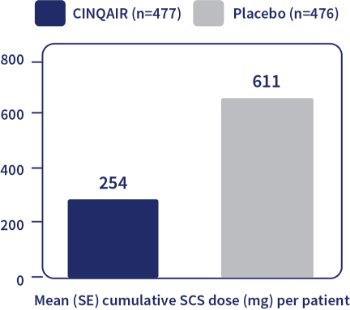
OCSs=oral (systemic) corticosteroids.
Reduction in exacerbations
requiring OCSs
- Study I: 55% reduction in exacerbations requiring OCSs
Study Design: Studies I-II1,2
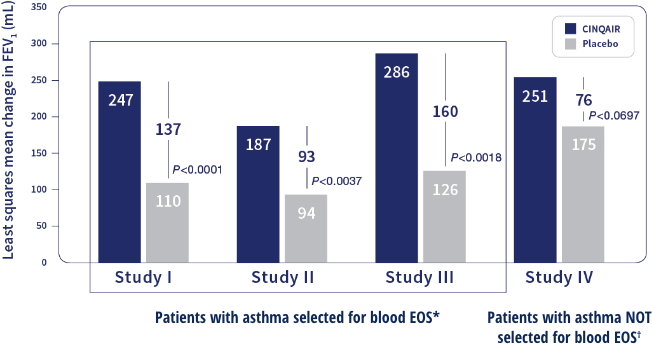
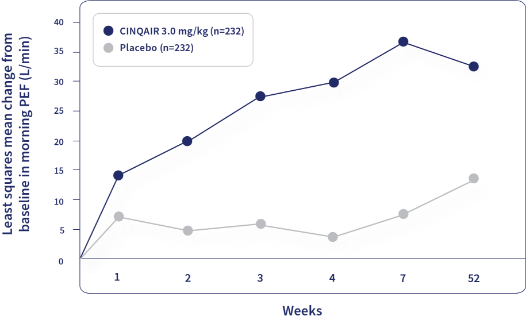
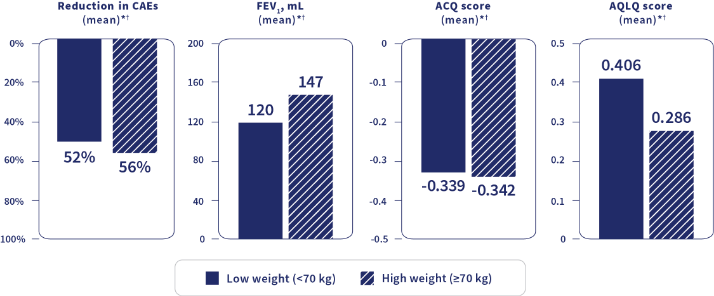
Design: 52-week studies comparing treatment with CINQAIR or placebo along with background asthma therapy in 953 patients with severe asthma who were required to have a blood eosinophil count ≥400/mcL (within 3-4 weeks of dosing) and ≥1 asthma exacerbation requiring systemic corticosteroid use over the past 12 months. The majority of patients were on medium-high dose inhaled corticosteroids (ICSs) plus a long-acting beta agonist (LABA) at baseline. Maintenance OCSs were allowed. Primary Endpoint: Frequency of asthma exacerbations. Secondary Endpoints: Change from baseline in forced expiratory volume in one second (FEV1), blood eosinophil count, Asthma Control Questionnaire-7 (ACQ-7) score, and Asthma Quality of Life Questionnaire (AQLQ) total score. Exacerbation Definition: A worsening of asthma that required at least 1 of the following medical interventions: 1) Either the use of a systemic corticosteroid (if not already taking), or a ≥2-fold increase in the use of ICSs for 3 or more days, and/or 2) Asthma-related emergency treatment including at least 1 of the following: an unscheduled visit to their healthcare professional for nebulizer treatment or other urgent treatment to prevent worsening of asthma symptoms; a visit to the emergency room for asthma-related treatment; or an asthma-related hospitalization.